Nanocomposite Hydrogels Offer Extended Drug Delivery
Nanocomposite Hydrogels Offer Extended Drug Delivery


Researchers at Stanford University have developed a novel hydrogel depot to reduce the number of injections required for those living with Type 2 diabetes.
According to the Centers for Disease Control and Prevention (CDC), more than 38 million Americans live with diabetes. Most of them have been diagnosed with the Type 2 variety, where the body, over time, becomes resistant to insulin, a hormone needed to transform the carbohydrates in food into cellular energy.
Fortunately, within the last few years, new diabetes drugs have come on the market that target glucagon-like peptide 1 (GLP-1), a hormone that stimulates insulin secretion. These medications have been game changers for many patients, helping them not only lower their hemoglobin A1C levels, a standard measure of blood glucose, but also facilitate weight loss and smarter dietary choices. There’s only one downside: most of these drugs require weekly or even daily injections.
“Drug adherence is a big issue with Type 2 diabetes management,” said Andrea d’Aquino, a postdoctoral fellow in the department of materials science and engineering at Stanford University. “These frequent injections can be a significant patient burden and keep them from taking the medications that can help them better manage their disease.”
To reduce that burden, d’Aquino, along with Eric Appel, associate professor of materials science and engineering, decided to develop a novel hydrogel depot so that patients would only need to inject themselves with GLP-1 drugs a few times a year, lined up to their regularly scheduled endocrinology appointments.
Dissolving Devices: Stamp-Like Device Treats Heart Disease, Then Dissolves
“Hydrogels have been around forever—and synthetic gels have been evaluated as a potential drug delivery vehicle for decades. We know they are very biocompatible,” said Appel. “But we wanted to create a new type of gel that would be easy to manufacture and stable enough that you could inject it with a standard pen injector the same way that patients already do with their current diabetes medications.”
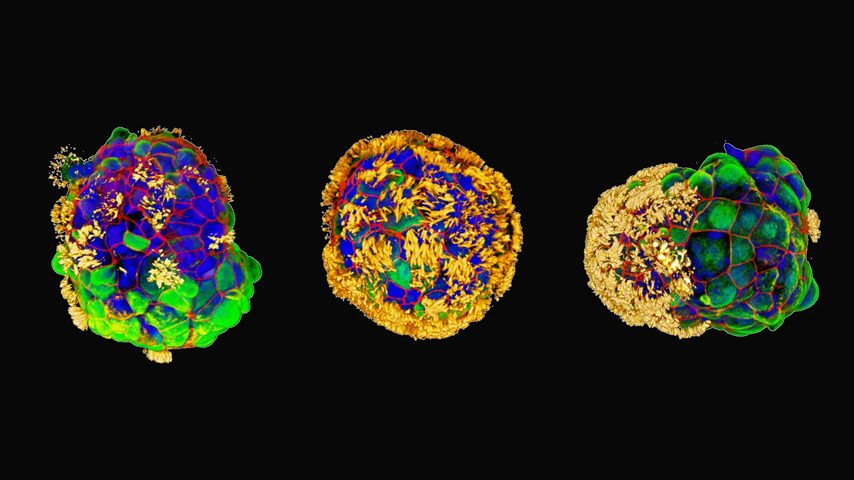
Others have attempted to develop hydrogel-based depot technology for pharmaceutical products but have been unable to come up with a specific formula that meets all safety and regulatory standards. But d’Aquino, Appel, and colleagues took a different approach from those in the past: they looked to bond polymers in their hydrogel non-covalently.
“We use an approach that we call molecular Velcro. There’s a special interaction between the polymer chains and nanoparticles so they are weekly bound together. The polymer chains are cross-linked together to make a mesh that can hold the drug—but while they are chemically bonded, they aren’t physically stuck together,” Appel explained.
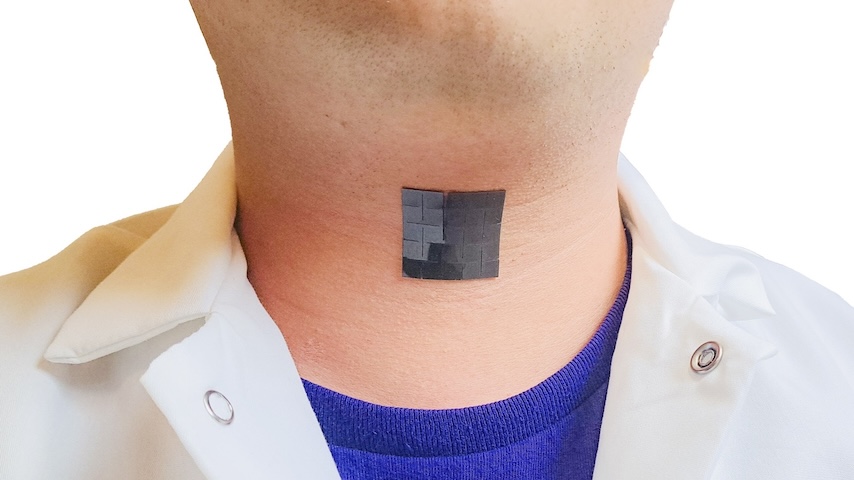
The result is a polymer-nanoparticle (PNP) hydrogel, where GLP-1 drugs can be formulated directly into the gel itself. When the payload is injected under the skin, much in the same way one of the GLP-1 drugs are injected today, it dissolves away over time, leading to a controlled release of the drug.
Become a Member: How to Join ASME
“In this case, you have the depot with the drug, and it just dissolves the same way a lump of sugar would dissolve in water,” said Appel. “That process of dissolution is what delivers the drug. So, the depot gets smaller and smaller over time until it disappears.”
One of the biggest challenges in developing the PNP hydrogel was finding the right balance of control, or creating a depot that was small enough to not bother patients and could remain in the body, slowly releasing the drug over a specified amount of time.
“Trying to create something that will stay consistently in the body for the amount of time you choose and precisely maintain the exposure to a certain drug is complex and multifaceted,” Appel said. “We opted to deliver the drug over four months, because, generally, patients meet with their doctor every four months.”
In laboratory tests, the formulation worked. In a study published in Cell Reports Medicine, the team demonstrated they were able to fine-tune the release of the GLP-1 drug over a four-month period. When the researchers tested the hydrogel depot on laboratory rats, they saw their delivery device improved management of blood glucose, as well as weight, compared to the animals receiving daily injections of the same drug. The researchers hope to take the hydrogel into clinical trials within the next few years. Appel added that it should be fairly easy to scale this technology for manufacturing.
Drug Delivery in Space: Injecting Medicine in Zero Gravity
“This hydrogel has two components: a polymer and a nanoparticle. Because this molecular Velcro is like a protein and ligand with a very specific interaction, you can mix them together and thermodynamics really does the work to create the gel,” he said. “And the same way that the gel is fluid enough to be injectable, it’s also pumpable, which means you could mix the components in a large vat and fill up a bunch of pen injectors. The properties that allow for simple mixing and pumping make it ideal for manufacturing.”
In terms of next steps, d’Aquino said she and her colleagues are interested in creating new gels for other drugs, as well as gels that support different release times. And as they continue to work on this unique hydrogel, she said she is buoyed by the fact that this kind of drug delivery system could significantly improve adherence in individuals living with Type 2 diabetes in the future.
“This could reduce patient burden and, as a result, improve patient outcomes,” she said. “This could be really transformative for patients’ lives. But it’s likely there are also many other patients with chronic conditions who could benefit from this technology too and we plan to look at other diseases like Type 1 diabetes to see how we can use these gels to make it easier for them to take their medications.”
Kayt Sukel is a technology writer and author in Houston.