Pacemaker Powered by Optical Fiber
Pacemaker Powered by Optical Fiber
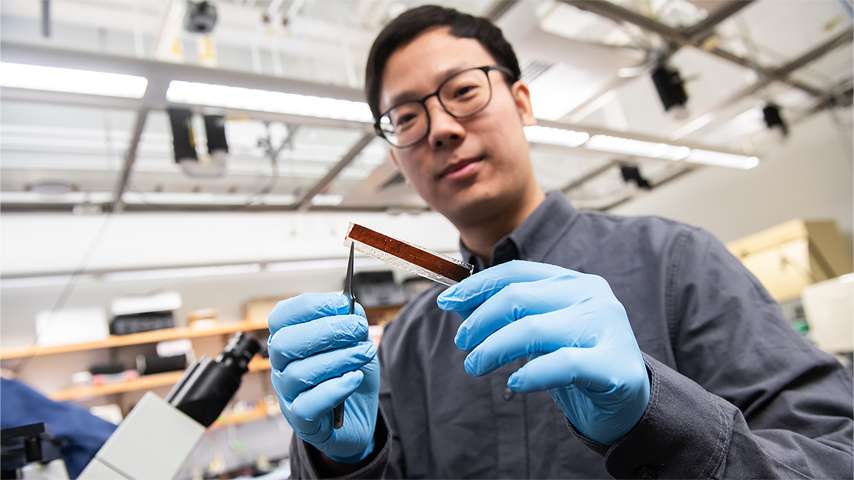
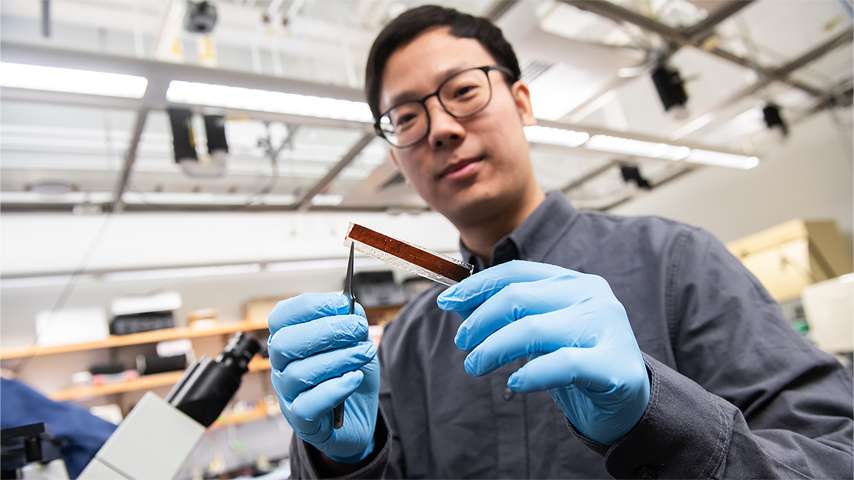
Photovoltaic cell on a medical implant harvests light from a hair-thin cable to provide essential cardiac stimulation. Researcher Pengju Li holds the material. Photo by Jean Lachat
Pacemakers can be lifesavers for patients diagnosed with heart arrhythmias. About a million of these small devices, made up of electrodes to sense your natural heartbeat as well as a pulse generator with a battery and leads to stimulate the heart to get an irregular rhythm back on track, are implanted worldwide each year, according to the National Institutes of Health. But some patients have difficulties with them. They have too many moving parts which can lead to issues.
Bozhi Tian, professor of Chemistry at the University of Chicago whose research specializes in the development of photovoltaic biomedical devices, said making them smaller and less intrusive would be beneficial for patients. “Traditional cardiac pacemakers only have one or two leads – that’s the typical configuration,” he said. “That means there are only one or two electrodes to stimulate the heart. Let’s say, over time, the optimal stimulation condition or the location of those electrodes has to be modified. Unless you do an additional surgery, it’s very challenging to modify things and that can lead to complications.”
Now, Tian and colleagues have created a new ultra-thin material, powered by light, which can address this issue. The flexible, micrometer thin membrane, which the researchers call a photoelectroceutical, weighs less than one fiftieth of a gram. It can be non-invasively implanted into the heart and controlled with an optic fiber. Tian said inspiration for the design of the groundbreaking device comes from the retina.
“If you think about how the retina receives the light, it’s really random access,” he said. “If you have a very small spot of light, and it only hits a certain portion of the retina, only the photoreceptor cells in that area will respond to it. If you move that spot of light to a different area of the retina, that portion of photoreceptor cells can also receive it. In our design with this device, we moved to mimic biology, and achieve random access photo stimulation so that we could use light to define the location for the electrical stimulation and activate only that area.”
Discover the benefits of ASME membership
The resulting design, which has two layers of P-type silicon material, creates an electrical charge when it is exposed to light. The top layer is nanoporous, which enables it to concentrate the charge without allowing it to spread. The researchers said the design means they can easily and temporarily insert the device, along with an optic fiber, in a non-invasive manner. The optic fiber is programmed to light up in a specific pattern. The membrane can then picks up those signals from the fiber and translate them into electrical impulses to stimulate heart tissue.
“The optic fiber we use is very thin – and the tail of the optic fiber can run from the heart to the surface of the skin,” he said. “The other end can then be connected to an LED (light emitting diode) device to provide the light. We do not need strong or intense light, either. A commercially available LED device is good enough. We could also potentially implant an LED under the skin, if the LED had wireless capabilities, so you could control it wirelessly to give it the pulse to stimulate the heart.”
In a series of experiments, the research group tested the membrane in heart tissue – and then on pig hearts. They were able to precisely stimulate the heart – achieving the desired random access photostimulation as desired.
While this unique pacemaker design is only meant for temporary use at this time—the material dissolves into non-toxic silicic acid within a few weeks—Tian said this approach holds great promise for future cardiac stimulation devices. The research group is already at work to commercialize the device so it can eventually move from the laboratory to the clinic. Tian said he and his colleagues are collaborating with cardiac surgeons to launch a start-up company to help with that endeavor.
He added that he and his team also see the potential of using this kind of approach for stimulating brain tissue for neuromodulatory applications. For example, photoelectroceuticals could be used to stimulate neurons in neurodegenerative disorders like Parkinson’s disease or to help manage chronic pain.
More biomedical breakthroughs: Wearable Patch Offers Voice to the Voiceless
But, Tian said, to get to that point, there is still a great deal of engineering work left to do, that’s just to improve it for the temporary pacemaker application.
“We must still improve the device performance and stability inside the body,” he said. “Right now, our design is for an acute cardiac stimulation application. We only ran our experiment for about three hours. For three hours, the device worked perfectly. But for many of these other applications, we want it to last for one month, or perhaps even longer. We need to make sure we are designing in a way that the device is stable. We also need to optimize the device’s stimulation delivery configuration and its efficiency. There is still a lot of work to do.”
Kayt Sukel is a technology and business writer in Houston.
Bozhi Tian, professor of Chemistry at the University of Chicago whose research specializes in the development of photovoltaic biomedical devices, said making them smaller and less intrusive would be beneficial for patients. “Traditional cardiac pacemakers only have one or two leads – that’s the typical configuration,” he said. “That means there are only one or two electrodes to stimulate the heart. Let’s say, over time, the optimal stimulation condition or the location of those electrodes has to be modified. Unless you do an additional surgery, it’s very challenging to modify things and that can lead to complications.”
Now, Tian and colleagues have created a new ultra-thin material, powered by light, which can address this issue. The flexible, micrometer thin membrane, which the researchers call a photoelectroceutical, weighs less than one fiftieth of a gram. It can be non-invasively implanted into the heart and controlled with an optic fiber. Tian said inspiration for the design of the groundbreaking device comes from the retina.
“If you think about how the retina receives the light, it’s really random access,” he said. “If you have a very small spot of light, and it only hits a certain portion of the retina, only the photoreceptor cells in that area will respond to it. If you move that spot of light to a different area of the retina, that portion of photoreceptor cells can also receive it. In our design with this device, we moved to mimic biology, and achieve random access photo stimulation so that we could use light to define the location for the electrical stimulation and activate only that area.”
Discover the benefits of ASME membership
The resulting design, which has two layers of P-type silicon material, creates an electrical charge when it is exposed to light. The top layer is nanoporous, which enables it to concentrate the charge without allowing it to spread. The researchers said the design means they can easily and temporarily insert the device, along with an optic fiber, in a non-invasive manner. The optic fiber is programmed to light up in a specific pattern. The membrane can then picks up those signals from the fiber and translate them into electrical impulses to stimulate heart tissue.
“The optic fiber we use is very thin – and the tail of the optic fiber can run from the heart to the surface of the skin,” he said. “The other end can then be connected to an LED (light emitting diode) device to provide the light. We do not need strong or intense light, either. A commercially available LED device is good enough. We could also potentially implant an LED under the skin, if the LED had wireless capabilities, so you could control it wirelessly to give it the pulse to stimulate the heart.”
In a series of experiments, the research group tested the membrane in heart tissue – and then on pig hearts. They were able to precisely stimulate the heart – achieving the desired random access photostimulation as desired.
While this unique pacemaker design is only meant for temporary use at this time—the material dissolves into non-toxic silicic acid within a few weeks—Tian said this approach holds great promise for future cardiac stimulation devices. The research group is already at work to commercialize the device so it can eventually move from the laboratory to the clinic. Tian said he and his colleagues are collaborating with cardiac surgeons to launch a start-up company to help with that endeavor.
He added that he and his team also see the potential of using this kind of approach for stimulating brain tissue for neuromodulatory applications. For example, photoelectroceuticals could be used to stimulate neurons in neurodegenerative disorders like Parkinson’s disease or to help manage chronic pain.
More biomedical breakthroughs: Wearable Patch Offers Voice to the Voiceless
But, Tian said, to get to that point, there is still a great deal of engineering work left to do, that’s just to improve it for the temporary pacemaker application.
“We must still improve the device performance and stability inside the body,” he said. “Right now, our design is for an acute cardiac stimulation application. We only ran our experiment for about three hours. For three hours, the device worked perfectly. But for many of these other applications, we want it to last for one month, or perhaps even longer. We need to make sure we are designing in a way that the device is stable. We also need to optimize the device’s stimulation delivery configuration and its efficiency. There is still a lot of work to do.”
Kayt Sukel is a technology and business writer in Houston.





