Contact Lens Shifts Focus in Fight Against Glaucoma
Contact Lens Shifts Focus in Fight Against Glaucoma
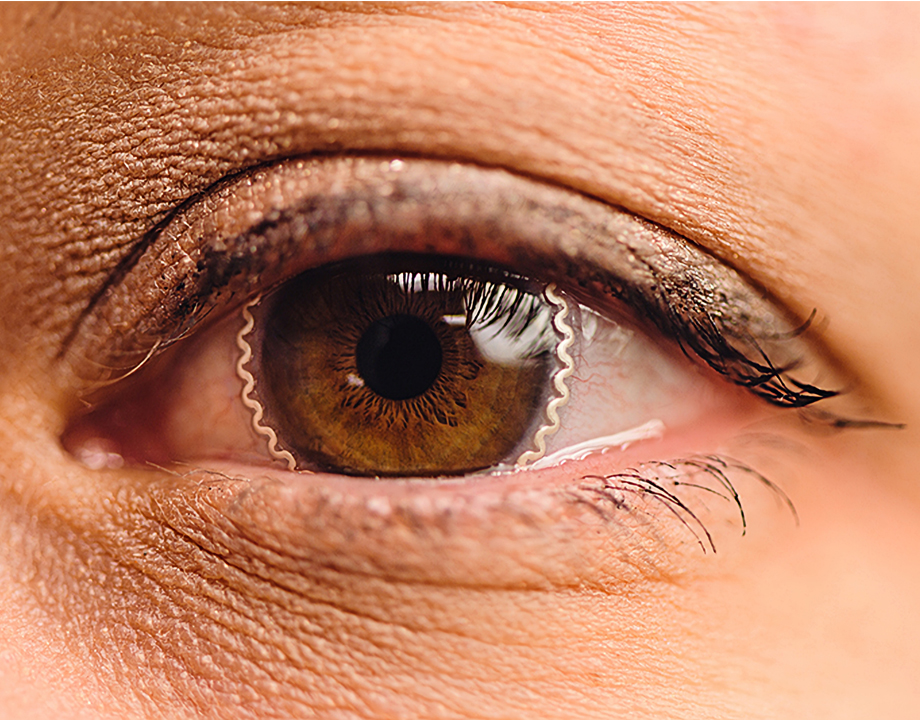
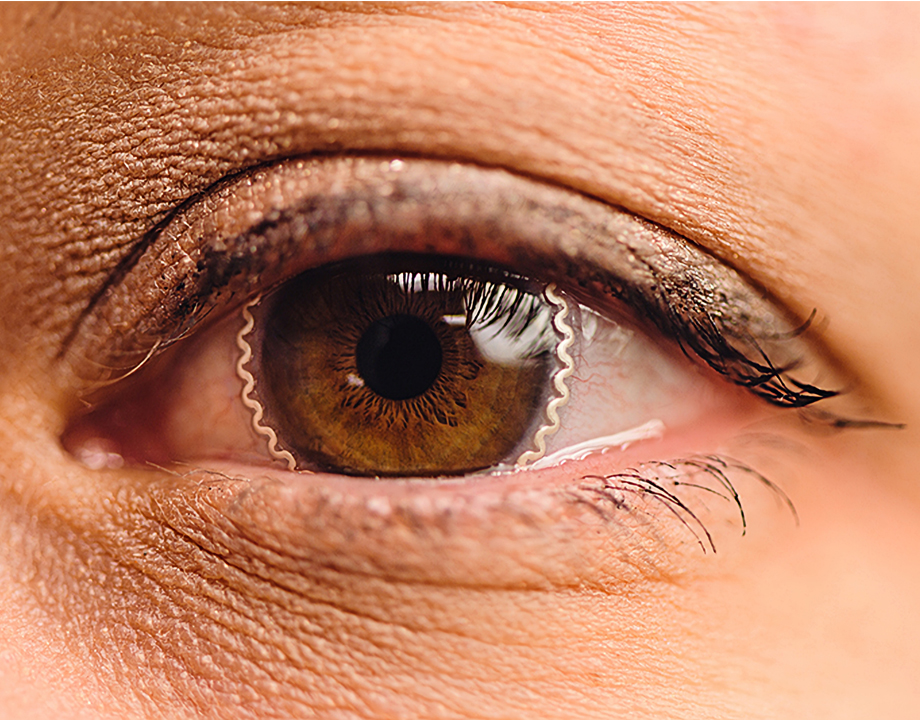
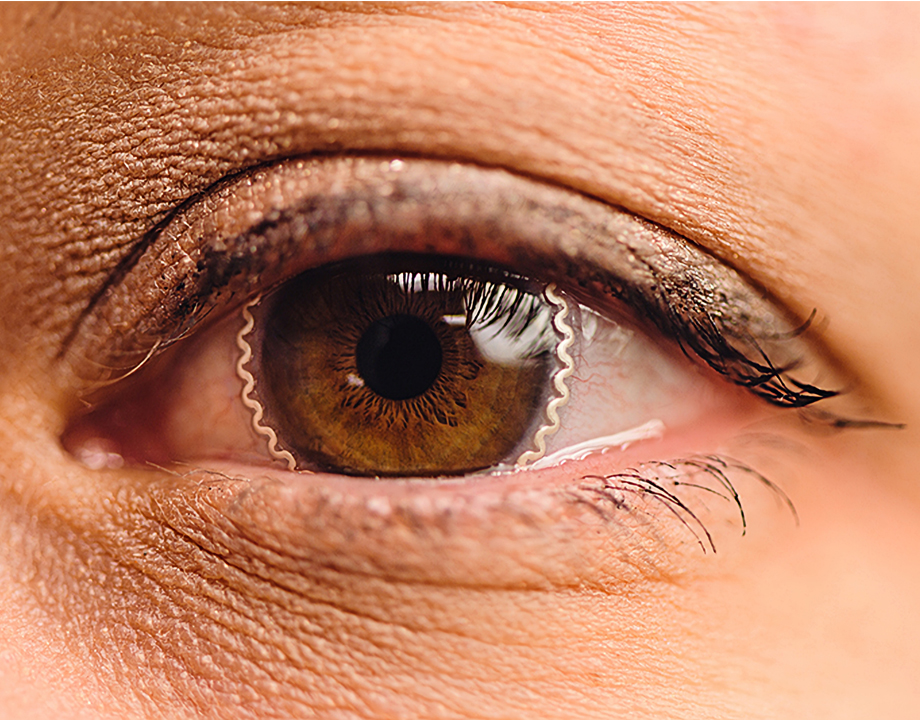
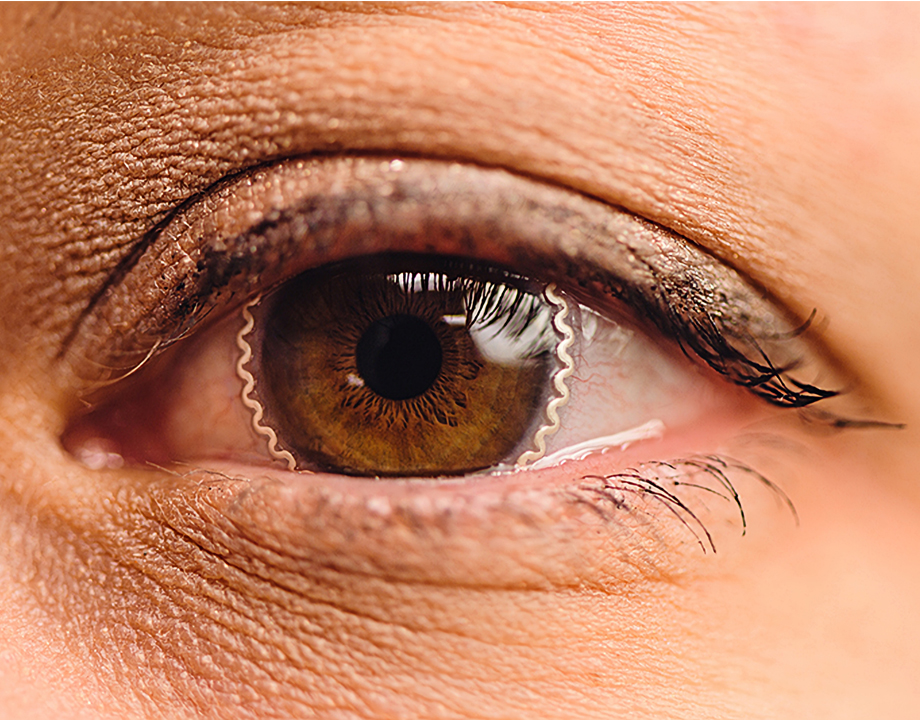
New wearable biomedical lens could help save the eyes of millions of people by continuously monitoring intraocular pressure (IOP)—even during sleep—sparing them from sight-robbing Glaucoma.
A new cop in town could soon be on the job day and night with the mission of arresting the silent thief of sight, glaucoma.
This cop comes in the form of a soft, comfortable contact lens that continuously monitors intraocular pressure (IOP) and alerts the wearer when IOP increases. Glaucoma, a top cause of blindness worldwide, gradually robs people of their eyesight, often without early warning signs. Immediately lowering pressure in the inner eye can help slow glaucoma’s progress and prevent ongoing damage.
Chi Hwan Lee, the Leslie Geddes Associate Professor of Biomedical Engineering and associate professor of mechanical engineering at Purdue University, embarked on the research, recently published in Nature Communications, knowing how difficult it is to monitor IOP over long periods of time, especially when a person is sleeping. It’s the type of project he said young researchers increasingly gravitate toward.
More Like This: Mechanical Engineers Prepare MIRA for the Next Frontier
“My mechanical engineering students want to understand how to leverage their own experience while collaborating with different groups to tackle a big-picture problem,” Lee said, noting that glaucoma affects nearly 80 million people worldwide. “Improving human health is one of the biggest problems we need to tackle.”
Lee, whose work focuses on wearable biomedical devices and the mechanics and materials for flexible electronics, began thinking of his lens after reading about a joint venture between Google X and pharma giant Novartis in 2014 to develop a smart contact lens to help people with diabetes by measuring glucose levels in tears. A tiny sensor, computer chip, and antenna were embedded on the side of the lens and sandwiched between two contact lens layers. Novartis reportedly backed out of the partnership in 2017 after questioning the reliability of measuring glucose levels through tears.
Lee recognized another big problem with the lens, this one having to do with design. Based on his experience with flexible electronics, he believed the material of the Google lens would be too rigid to provide a comfortable, seamless, ergonomic fit, and allow for proper oxygen transmissibility, among other issues. Tonometers, the sensor that measures IOP in many of today’s wearable ocular devices, also add unwanted thickness, stiffness, and blurriness to the lens.
More of Interest for You: New Surface Coating for Medical Devices Prevents Hospital Infections
“All of those problems need to be addressed or people will not use the lens,” Lee said. A reliable and accurate home technology, he added, would remotely gather sufficient information to help specialists provide optimal treatment and limit visits to a doctor.
When it came to correcting many of the issues, Lee realized he didn’t have to reinvent the wheel. Instead, he started off with commercial brands of soft contact lenses and other materials already used in biomedical devices. That approach helps to lower the hurdle for gaining Food and Drug Administration approval.
The research team, a multidisciplinary group of engineers and health researchers from Purdue’s colleges of engineering and veterinary medicine and the Indiana University School of Optometry, faced several mechanical challenges enroute to a finished lens.
To create a comfortable and sturdy tonometer, Lee relied on a unique method of applying a very thin sensor and antenna to the lens. Soft contacts are made from hydrogels that are typically 80 to 90 percent water, making them incredibly slippery and fragile, something Lee wasn’t entirely aware of since he doesn’t wear contacts.
When collaborators at the school of optometry tried to handle an early prototype the way they would a regular contact lens, it fell apart. The tonometer layer, Lee realized, had to be made from a material at least 10 times more stretchable than the soft lens attached to it.
Lee hit the drawing board, relying on experience creating flexible materials in his “sticktronics” lab. Sticktronics, a term Lee coined, refers to smart films embedded with high-performance electronics and sensors that are pealed from a backing and stuck to another object to provide unique functionality. He ended up developing a very soft, stretchable elastomer made from polydimethylsiloxane for encapsulation, polystyrene embedded with silver flakes for conductivity, and Silbione liquid rubber for a highly compressible interlayer.
Related Content: Wearable Muscles Work with Users to Restore Mobility
The next challenge was finding an adhesive that could permanently bond to an incredibly wet and slippery surface. For that, he and a chemical engineer turned to mussels. The mollusk clings to wet objects, even in fierce currents, thanks to foot proteins containing polydopamine adhesive (PDA). Lee synthesized a similar PDA. He found his bond and used it to create a soft, sturdy lens that deforms with the cornea when IOP pressure changes. The information wirelessly transmits to a reader coil attached to a pair of eyeglasses or a sleeping mask.
The coil is attached to an analyzer (a standalone device at night or a smartphone) that warns the wearer of sudden pressure change. It also sends information to a cloud server, where a doctor or clinician can retrieve it. Lees said there are several devices on the market that measure IOP during the day, but not during sleep. IOP changes constantly, but it has a much higher chance of increasing while a person is lying down, Lee said.
Sign up: ASME Membership Benefits
Lee recently developed a startup company and is working with Boomerang Ventures in Indianapolis to raise funding for large clinical trials, the creation of an app, further validation, and ongoing improvements. Human subjects in a small initial trial said the lens was comfortable and did not affect their vision. Lee attributes that success to his diverse team.
“All of the different mechanical engineering components we used, along with the different disciplines on the team, are critical in tackling this big problem and translating the basic research into a real-world application,” he said.
Jeff O’Heir is a science and technology writer based in Huntington, NY.
This cop comes in the form of a soft, comfortable contact lens that continuously monitors intraocular pressure (IOP) and alerts the wearer when IOP increases. Glaucoma, a top cause of blindness worldwide, gradually robs people of their eyesight, often without early warning signs. Immediately lowering pressure in the inner eye can help slow glaucoma’s progress and prevent ongoing damage.
Chi Hwan Lee, the Leslie Geddes Associate Professor of Biomedical Engineering and associate professor of mechanical engineering at Purdue University, embarked on the research, recently published in Nature Communications, knowing how difficult it is to monitor IOP over long periods of time, especially when a person is sleeping. It’s the type of project he said young researchers increasingly gravitate toward.
More Like This: Mechanical Engineers Prepare MIRA for the Next Frontier
“My mechanical engineering students want to understand how to leverage their own experience while collaborating with different groups to tackle a big-picture problem,” Lee said, noting that glaucoma affects nearly 80 million people worldwide. “Improving human health is one of the biggest problems we need to tackle.”
Lee, whose work focuses on wearable biomedical devices and the mechanics and materials for flexible electronics, began thinking of his lens after reading about a joint venture between Google X and pharma giant Novartis in 2014 to develop a smart contact lens to help people with diabetes by measuring glucose levels in tears. A tiny sensor, computer chip, and antenna were embedded on the side of the lens and sandwiched between two contact lens layers. Novartis reportedly backed out of the partnership in 2017 after questioning the reliability of measuring glucose levels through tears.
Lee recognized another big problem with the lens, this one having to do with design. Based on his experience with flexible electronics, he believed the material of the Google lens would be too rigid to provide a comfortable, seamless, ergonomic fit, and allow for proper oxygen transmissibility, among other issues. Tonometers, the sensor that measures IOP in many of today’s wearable ocular devices, also add unwanted thickness, stiffness, and blurriness to the lens.
More of Interest for You: New Surface Coating for Medical Devices Prevents Hospital Infections
“All of those problems need to be addressed or people will not use the lens,” Lee said. A reliable and accurate home technology, he added, would remotely gather sufficient information to help specialists provide optimal treatment and limit visits to a doctor.
When it came to correcting many of the issues, Lee realized he didn’t have to reinvent the wheel. Instead, he started off with commercial brands of soft contact lenses and other materials already used in biomedical devices. That approach helps to lower the hurdle for gaining Food and Drug Administration approval.
The research team, a multidisciplinary group of engineers and health researchers from Purdue’s colleges of engineering and veterinary medicine and the Indiana University School of Optometry, faced several mechanical challenges enroute to a finished lens.
To create a comfortable and sturdy tonometer, Lee relied on a unique method of applying a very thin sensor and antenna to the lens. Soft contacts are made from hydrogels that are typically 80 to 90 percent water, making them incredibly slippery and fragile, something Lee wasn’t entirely aware of since he doesn’t wear contacts.
When collaborators at the school of optometry tried to handle an early prototype the way they would a regular contact lens, it fell apart. The tonometer layer, Lee realized, had to be made from a material at least 10 times more stretchable than the soft lens attached to it.
Lee hit the drawing board, relying on experience creating flexible materials in his “sticktronics” lab. Sticktronics, a term Lee coined, refers to smart films embedded with high-performance electronics and sensors that are pealed from a backing and stuck to another object to provide unique functionality. He ended up developing a very soft, stretchable elastomer made from polydimethylsiloxane for encapsulation, polystyrene embedded with silver flakes for conductivity, and Silbione liquid rubber for a highly compressible interlayer.
Related Content: Wearable Muscles Work with Users to Restore Mobility
The next challenge was finding an adhesive that could permanently bond to an incredibly wet and slippery surface. For that, he and a chemical engineer turned to mussels. The mollusk clings to wet objects, even in fierce currents, thanks to foot proteins containing polydopamine adhesive (PDA). Lee synthesized a similar PDA. He found his bond and used it to create a soft, sturdy lens that deforms with the cornea when IOP pressure changes. The information wirelessly transmits to a reader coil attached to a pair of eyeglasses or a sleeping mask.
The coil is attached to an analyzer (a standalone device at night or a smartphone) that warns the wearer of sudden pressure change. It also sends information to a cloud server, where a doctor or clinician can retrieve it. Lees said there are several devices on the market that measure IOP during the day, but not during sleep. IOP changes constantly, but it has a much higher chance of increasing while a person is lying down, Lee said.
Sign up: ASME Membership Benefits
Lee recently developed a startup company and is working with Boomerang Ventures in Indianapolis to raise funding for large clinical trials, the creation of an app, further validation, and ongoing improvements. Human subjects in a small initial trial said the lens was comfortable and did not affect their vision. Lee attributes that success to his diverse team.
“All of the different mechanical engineering components we used, along with the different disciplines on the team, are critical in tackling this big problem and translating the basic research into a real-world application,” he said.
Jeff O’Heir is a science and technology writer based in Huntington, NY.