Powerless Air Blender Breathes Life
Powerless Air Blender Breathes Life
A simple syringe is the inspiration behind a new medical device that is a low-cost alternative to expensive CPAP machines.
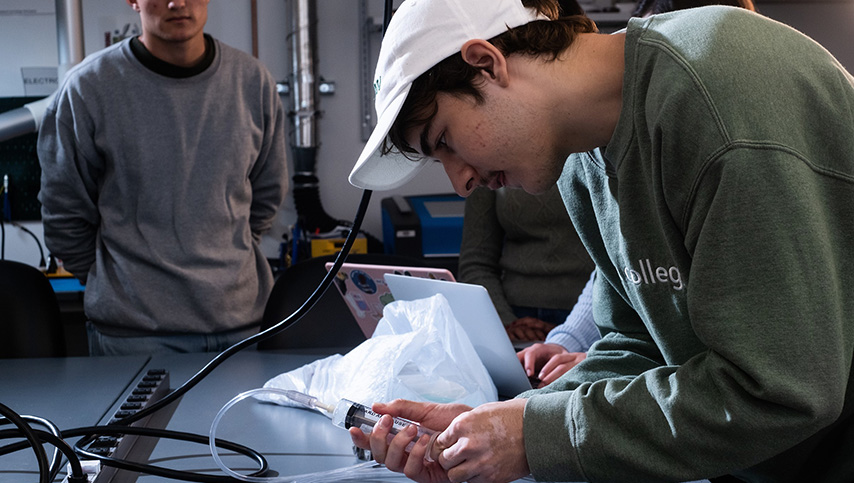
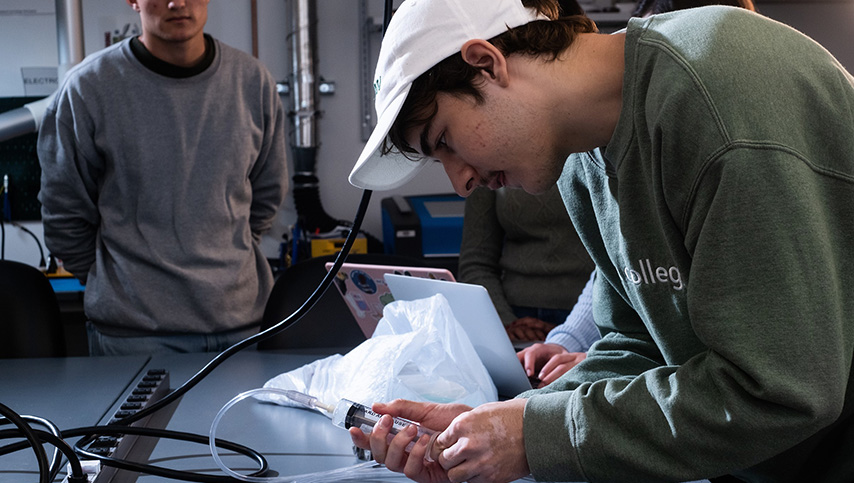
What began as a class assignment is now a tool that solves a critical health care problem. This medical device was developed by a team of Rice University students to blend oxygen and air and deliver life-saving respiratory support to premature babies in low-resource locations.
The four-person team—self-dubbed “Avatar The Last Air Blender” in homage to the quite fitting animated series—united during a Global Health 360 class at Rice University’s Oshman Engineering Design Kitchen (OEDK) with the goal of developing a simple, inexpensive air blender that could work without power.
“I get a mix of bioengineers and non-bioengineers, and I really emphasize you're not limited to what you came in with. The bioengineers don't get to do all of the engineering, and the non-bioengineers don't have to do all of the writing,” explained Meaghan Bond, the group’s mentor and professor at the Richards-Kortum Optical Spectroscopy and Imaging Laboratory at Rice. “They're able to cross those disciplines and learn new skills.”
The team is comprised of bioengineering majors Harlan Cook and Brennan Keogh, both rising seniors, with biosciences major Leora Maksoud and anthropology major Ojas Dumbre, both rising juniors. A Global Health 360 class focused on neonatal care in low-resource settings presented the oxygen blending issue to the team, matching them with a health care mentor, neonatologist Chiamaka Aneji, in the Texas Medical Center, and engineering mentor, Madeleine Weld, an engineer at Rice360.
“Obviously, we're doing this project in the United States, but we want to understand the perspective of like people living in sub-saharan Africa or other low-resource settings and not assume what we think would be happening in those hospitals, but really what the physicians and the engineers are saying,” Dumbre said.
“We thought, this is perfect—it doesn’t use power,” Cook said. “The paper mentioned how changing the distance between the jet nozzle and the outlet orifice would change the oxygen concentration. We thought, what are ways that we can linearly move the Venturi back and forth, and Ojas said, what about a syringe?”
You Might Also Enjoy: Tattooed on the Heart
Using a standard 60 ml syringe as inspiration, the team designed and 3D-printed their prototype. Within the syringe tube is a modified plunger with a hollow tube in it that allows pure oxygen to pass through the syringe tube, Cook explained. At the end of the tube is a Venturi jet that reduces the diameter of the tube, speeding up the air in the process.
“The air speeding up actually causes a pressure drop in this area, so we've cut a hole in that area in the syringe to allow outside air to come in,” he said. “So, when the pressure drops, it pulls in outside air, which blends with the oxygen and that's what the patient receives.”
By moving the jet back and forth, the user will change the jet distance, thus altering the amount of outside air blending with oxygen. “So, when it's really close to this orifice, you get a high concentration, and as you move it further back, you get lower and lower concentrations,” Cook said. In its current state, the device can blend oxygen in specific amounts from 95 percent to 30 percent by simply adjusting the jet distance.
In high resource settings, that support is usually provided with CPAP machines that mix oxygen and air to deliver the proper mix to those babies, she said. But in low-resource settings, these kinds of oxygen air blending machines are highly inaccessible, with their high costs and dependence on electricity. Heath care providers will often turn to using pure oxygen on newborns, but this can lead to blindness and lung damage.
The team collaborated with Aneji to determine design criteria and identify goals for an air blending device.
Become a Member: How to Join ASME
One of those was ensuring that the device could deliver continuous custom oxygen concentrations. Another was ensuring that the device was as low cost as possible, with a goal of less than US$10 per unit.
Self-sufficiency, no reliance on electricity, and compatibility with any existing oxygen tubing were vital. “One of our other important criteria was durability,” Dumbre said. “That the device is able to withstand cleaning, sterilization, and will be able to function after many uses.”
Although some low-cost air blenders do exist, many remain largely inaccessible, Maksoud noted.
“In regard to the design process in global health, oftentimes the best solution is not necessarily the most complex, but rather it's the one that has most accurately identified the clinical need and most efficiently used the available resources to meet it,” she said. “In our case, the fact that we knew that this there were these low-cost air blenders available, but there is still this large gap in accessibility that led us to the syringe idea, which we thought would most effectively meet this problem of inaccessibility to devices that are available.”
“So the next step would be developing it further and fixing the flow rate issue, so that there's still enough air coming into the patient to function as a CPAP,” Cook said.
Toying with different types of printers and materials has helped to a degree. “We started out with filament deposit printers to try and print the tubing, but found there was a lot of back pressure, so the flow was quite low,” Keogh explained. “We went on to an SLA printer and we found much more success in making a nice clean inner tube. Since you're restricting the radius of that inner tube as air flows through it, any more friction or roughness inside that tube is going to contribute a lot to slowing down the flow rate.”
Health Care Innovations: New Medical Adhesive Stops Uncontrolled Bleeding
Experimenting with different parameters for the Venturi jet, different angles, diameter nozzle, and materials showed improvements as well. Now that the school year has ended, this team’s work on the project has concluded. But their work will be evaluated over the next several months to determine the right path forward.
“The program continues to evaluate student projects as we go,” Bond said. “Some of them continue for another round of undergrads, some of them go to a post back fellowship where a graduate student works for a year or two focused on a particular project. It really varies.”
The hope is that development on this device will continue to uncover its full potential and that it will eventually be available for mass production and distribution to areas in need.
“Design for low-resource areas improves everybody's lives everywhere. It’s not just for low-resource areas,” Cook added. “These low-cost devices could help people here too.”
Louise Poirier is senior editor.

The four-person team—self-dubbed “Avatar The Last Air Blender” in homage to the quite fitting animated series—united during a Global Health 360 class at Rice University’s Oshman Engineering Design Kitchen (OEDK) with the goal of developing a simple, inexpensive air blender that could work without power.
“I get a mix of bioengineers and non-bioengineers, and I really emphasize you're not limited to what you came in with. The bioengineers don't get to do all of the engineering, and the non-bioengineers don't have to do all of the writing,” explained Meaghan Bond, the group’s mentor and professor at the Richards-Kortum Optical Spectroscopy and Imaging Laboratory at Rice. “They're able to cross those disciplines and learn new skills.”
The team is comprised of bioengineering majors Harlan Cook and Brennan Keogh, both rising seniors, with biosciences major Leora Maksoud and anthropology major Ojas Dumbre, both rising juniors. A Global Health 360 class focused on neonatal care in low-resource settings presented the oxygen blending issue to the team, matching them with a health care mentor, neonatologist Chiamaka Aneji, in the Texas Medical Center, and engineering mentor, Madeleine Weld, an engineer at Rice360.
“Obviously, we're doing this project in the United States, but we want to understand the perspective of like people living in sub-saharan Africa or other low-resource settings and not assume what we think would be happening in those hospitals, but really what the physicians and the engineers are saying,” Dumbre said.
How it works
Although ideas such as using batteries, compressed gas, or even air pumps to power the device arose during the brainstorming process, a lightbulb went off when the team came across a paper that mentioned using the Venturi effect.“We thought, this is perfect—it doesn’t use power,” Cook said. “The paper mentioned how changing the distance between the jet nozzle and the outlet orifice would change the oxygen concentration. We thought, what are ways that we can linearly move the Venturi back and forth, and Ojas said, what about a syringe?”
You Might Also Enjoy: Tattooed on the Heart
Using a standard 60 ml syringe as inspiration, the team designed and 3D-printed their prototype. Within the syringe tube is a modified plunger with a hollow tube in it that allows pure oxygen to pass through the syringe tube, Cook explained. At the end of the tube is a Venturi jet that reduces the diameter of the tube, speeding up the air in the process.
“The air speeding up actually causes a pressure drop in this area, so we've cut a hole in that area in the syringe to allow outside air to come in,” he said. “So, when the pressure drops, it pulls in outside air, which blends with the oxygen and that's what the patient receives.”
By moving the jet back and forth, the user will change the jet distance, thus altering the amount of outside air blending with oxygen. “So, when it's really close to this orifice, you get a high concentration, and as you move it further back, you get lower and lower concentrations,” Cook said. In its current state, the device can blend oxygen in specific amounts from 95 percent to 30 percent by simply adjusting the jet distance.
Uncovering a solution
Up to 95 percent of the 2.4 million premature babies born annually require respiratory support, according to the World Health Organization. “The leading cause of premature newborn death worldwide is respiratory distress syndrome,” added Maksoud.In high resource settings, that support is usually provided with CPAP machines that mix oxygen and air to deliver the proper mix to those babies, she said. But in low-resource settings, these kinds of oxygen air blending machines are highly inaccessible, with their high costs and dependence on electricity. Heath care providers will often turn to using pure oxygen on newborns, but this can lead to blindness and lung damage.
The team collaborated with Aneji to determine design criteria and identify goals for an air blending device.
Become a Member: How to Join ASME
One of those was ensuring that the device could deliver continuous custom oxygen concentrations. Another was ensuring that the device was as low cost as possible, with a goal of less than US$10 per unit.
Self-sufficiency, no reliance on electricity, and compatibility with any existing oxygen tubing were vital. “One of our other important criteria was durability,” Dumbre said. “That the device is able to withstand cleaning, sterilization, and will be able to function after many uses.”
Although some low-cost air blenders do exist, many remain largely inaccessible, Maksoud noted.
“In regard to the design process in global health, oftentimes the best solution is not necessarily the most complex, but rather it's the one that has most accurately identified the clinical need and most efficiently used the available resources to meet it,” she said. “In our case, the fact that we knew that this there were these low-cost air blenders available, but there is still this large gap in accessibility that led us to the syringe idea, which we thought would most effectively meet this problem of inaccessibility to devices that are available.”
Next steps
In just four months, the team went from assignment to prototyped and tested device. Although the oxygen concentrations can reliably be changed, there are still some issues with flow rate dropping.“So the next step would be developing it further and fixing the flow rate issue, so that there's still enough air coming into the patient to function as a CPAP,” Cook said.
Toying with different types of printers and materials has helped to a degree. “We started out with filament deposit printers to try and print the tubing, but found there was a lot of back pressure, so the flow was quite low,” Keogh explained. “We went on to an SLA printer and we found much more success in making a nice clean inner tube. Since you're restricting the radius of that inner tube as air flows through it, any more friction or roughness inside that tube is going to contribute a lot to slowing down the flow rate.”
Health Care Innovations: New Medical Adhesive Stops Uncontrolled Bleeding
Experimenting with different parameters for the Venturi jet, different angles, diameter nozzle, and materials showed improvements as well. Now that the school year has ended, this team’s work on the project has concluded. But their work will be evaluated over the next several months to determine the right path forward.
“The program continues to evaluate student projects as we go,” Bond said. “Some of them continue for another round of undergrads, some of them go to a post back fellowship where a graduate student works for a year or two focused on a particular project. It really varies.”
The hope is that development on this device will continue to uncover its full potential and that it will eventually be available for mass production and distribution to areas in need.
“Design for low-resource areas improves everybody's lives everywhere. It’s not just for low-resource areas,” Cook added. “These low-cost devices could help people here too.”
Louise Poirier is senior editor.

Pulse of the Profession: CAD in 2030
As we enter yet another new epoch of CAD innovation, the lines between design and manufacturing phases will continue to blur.





