Simple Electric Bandage Heals Chronic Wounds
Simple Electric Bandage Heals Chronic Wounds
Research funded by DARPA has produced a biocompatible bandage that applies a therapeutic current to persistent open sores.
Chronic wounds are open sores that heal slowly, if they heal at all. A familiar example is the type of sore that often accompanies diabetes, and which increases the risks of amputation and mortality for patients. All told, chronic wounds affect about 2 percent of the U.S. population.
Unfortunately, presently available treatments are often expensive, complex, and only moderately effective. Researchers are searching for a better way treat these wounds.
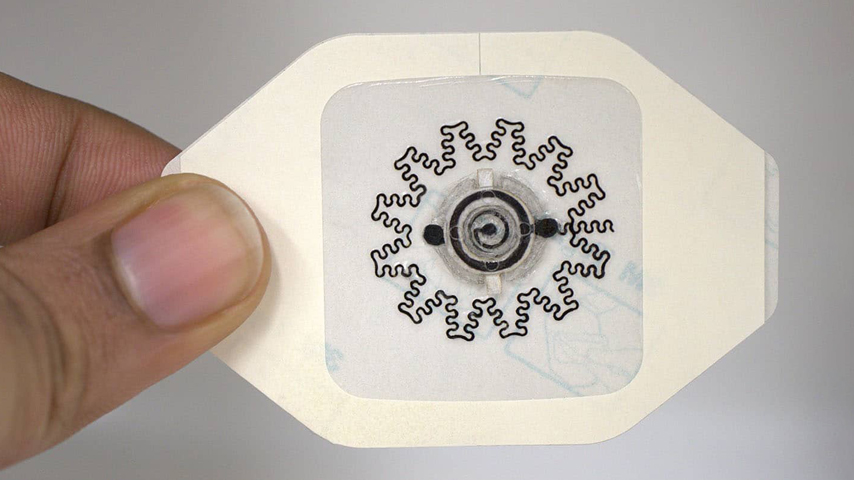
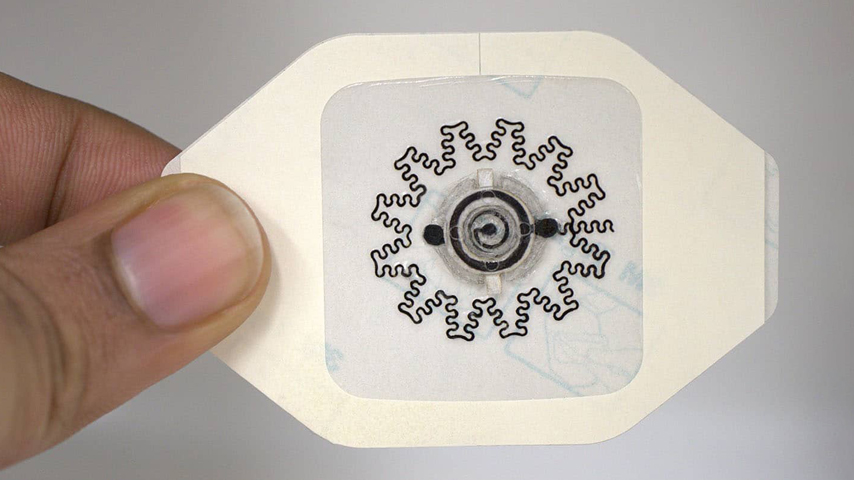
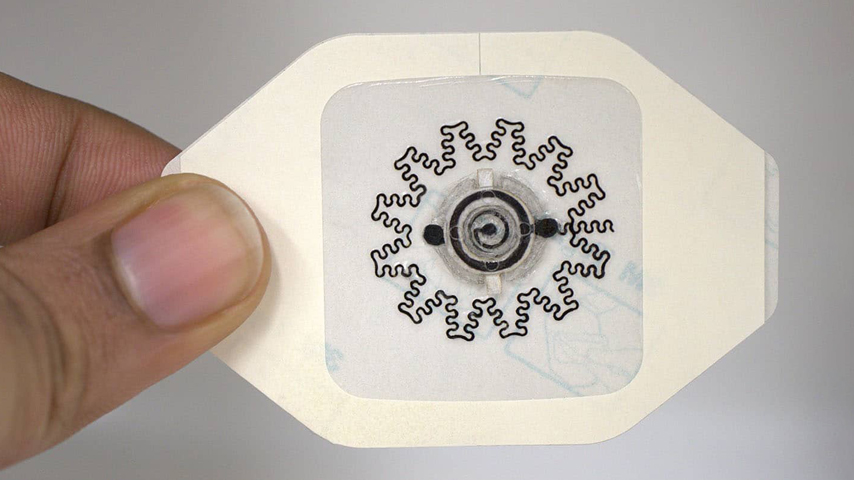
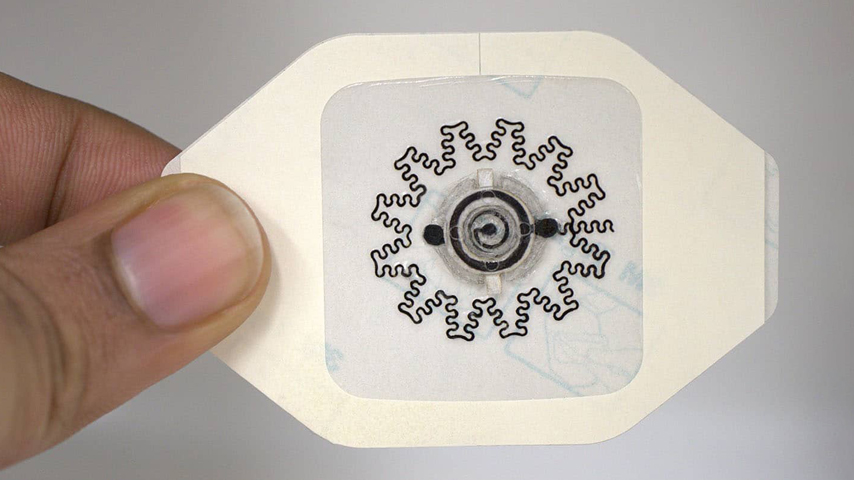
Recently, a international team of researchers funded with a grant from the Defense Advanced Research Projects Agency (DARPA) unveiled a new type of bandage that speeds the healing process. The disposable wound dressing has electrodes on one side and a small, biocompatible battery on the other. The application of a small but steady electric field was shown in tests to boost healing by 30 percent.
The project started in 2020, when Columbia University engineering professors Sam Sia and Ken Shepard won a $16.4 million grant from the Defense Advanced Research Projects Agency (DARPA) to develop a smart patch device to monitor and accelerate the wound-healing process. This research is part of a larger DARPA program that focuses on accelerated wound healing—especially for chronic wounds.
“Our goal with this grant is to develop a less-expensive technology that accelerates healing in patients with chronic wounds,” said Amay Bandodkar, an assistant professor of electrical and computer engineering at North Carolina State University and part of the research team. “We also wanted to make sure that the technology is easy enough for people to use at home, rather than something that patients can only receive in clinical settings.”
An “aha” moment occurred when Bandodkar attended a conference where he listened to several speakers talk about how many wound-care products were expensive and not that effective—and for wound-care products to be successful, they needed to be inexpensive, effective, and easy to use.
“At that time, we were working on new types of non-toxic batteries, and we started wondering if our batteries could somehow be embedded into bandages to provide pro-healing capabilities,” he said.
The research team that came together included experts from N.C. State, Columbia, Beth Israel Deaconess Medical Center, and the joint biomedical engineering program at N.C. State, University of North Carolina at Chapel Hill, Korea University, Georgia Tech, and the Korea Institute of Science and Technology. The project was supported by DARPA and co-led by Rajaram Kaveti (postdoc in Bandodkar’s lab) and Margaret Jakus (graduate student in Sia’s lab).
The team designed a water-powered, electronics-free dressing (WPED) that used a magnesium-silver chloride battery with a cellulose separator and a pair of stimulation electrodes. The addition of a small amount of water activates the battery, which creates a radial electric field, providing on-demand electrical stimulation for several hours. The WPED performs well, even under harsh conditions.
The dressing is applied to a patient so that the electrodes come into contact with the wound. The electrodes bend with the bandage and conform to the surface of the wound, which is often deep and irregularly shaped.
“This ability to conform is critical because we want the electric field to be directed from the periphery of the wound, toward the wound’s center,” Kaveti said. “In order to focus the electric field effectively, the electrodes need to be in contact with the patient at both the periphery and center of the wound itself. Since these wounds can be asymmetrical and deep, you need electrodes that can conform to a wide variety of surface features.”
“We tested the wound dressings in diabetic mice, which are a commonly used model for human wound healing,” Jakus added. “We found that the electrical stimulation from the device sped up the rate of wound closure, promoted new blood vessel formation, and reduced inflammation, all of which point to overall improved wound healing.”
 Specifically, the researchers discovered that mice who received treatment with WPEDs healed about 30 percent faster than mice who received conventional bandages. Across pre-clinical wound models, the WPED-treated group healed faster than the control, with wound closure rates comparable to treatments requiring expensive biologics or complex electronics.
Specifically, the researchers discovered that mice who received treatment with WPEDs healed about 30 percent faster than mice who received conventional bandages. Across pre-clinical wound models, the WPED-treated group healed faster than the control, with wound closure rates comparable to treatments requiring expensive biologics or complex electronics.
Bandodkar said that what surprised and pleased him the most about the research was the effectiveness of the electric field in the bandages.
“We were concerned that the unregulated electrical field generated by our bandage would not provide impressive healing outcomes,” he said. “Prior work on electrical field-based wound healing relied on well-regulated fields using bulky electronics. To our surprise, not only did our bandages accelerate healing, the healing rates of our low-cost bandages were comparable to those achieved using expensive biologics.”
Another key factor is that WPEDs can be produced at relatively low cost. “We’re talking about a couple of dollars per dressing in overhead costs,” said Bandodkar.
The bandages can also be applied quickly and easily—this functionality enables patients to treat themselves at home, meaning they will be more likely to comply with treatment.
“Next steps for us include additional work to fine-tune our ability to reduce fluctuations in the electric field and extend the duration of the field,” said Bandodkar. “We are also moving forward with additional testing that will get us closer to clinical trials and, ultimately, practical use that can help people.”
Mark Crawford is a technology writer in Corrales, N.M.
Unfortunately, presently available treatments are often expensive, complex, and only moderately effective. Researchers are searching for a better way treat these wounds.
Recently, a international team of researchers funded with a grant from the Defense Advanced Research Projects Agency (DARPA) unveiled a new type of bandage that speeds the healing process. The disposable wound dressing has electrodes on one side and a small, biocompatible battery on the other. The application of a small but steady electric field was shown in tests to boost healing by 30 percent.
The project started in 2020, when Columbia University engineering professors Sam Sia and Ken Shepard won a $16.4 million grant from the Defense Advanced Research Projects Agency (DARPA) to develop a smart patch device to monitor and accelerate the wound-healing process. This research is part of a larger DARPA program that focuses on accelerated wound healing—especially for chronic wounds.
“Our goal with this grant is to develop a less-expensive technology that accelerates healing in patients with chronic wounds,” said Amay Bandodkar, an assistant professor of electrical and computer engineering at North Carolina State University and part of the research team. “We also wanted to make sure that the technology is easy enough for people to use at home, rather than something that patients can only receive in clinical settings.”
An “aha” moment occurred when Bandodkar attended a conference where he listened to several speakers talk about how many wound-care products were expensive and not that effective—and for wound-care products to be successful, they needed to be inexpensive, effective, and easy to use.
“At that time, we were working on new types of non-toxic batteries, and we started wondering if our batteries could somehow be embedded into bandages to provide pro-healing capabilities,” he said.
The research team that came together included experts from N.C. State, Columbia, Beth Israel Deaconess Medical Center, and the joint biomedical engineering program at N.C. State, University of North Carolina at Chapel Hill, Korea University, Georgia Tech, and the Korea Institute of Science and Technology. The project was supported by DARPA and co-led by Rajaram Kaveti (postdoc in Bandodkar’s lab) and Margaret Jakus (graduate student in Sia’s lab).
The team designed a water-powered, electronics-free dressing (WPED) that used a magnesium-silver chloride battery with a cellulose separator and a pair of stimulation electrodes. The addition of a small amount of water activates the battery, which creates a radial electric field, providing on-demand electrical stimulation for several hours. The WPED performs well, even under harsh conditions.
The dressing is applied to a patient so that the electrodes come into contact with the wound. The electrodes bend with the bandage and conform to the surface of the wound, which is often deep and irregularly shaped.
“This ability to conform is critical because we want the electric field to be directed from the periphery of the wound, toward the wound’s center,” Kaveti said. “In order to focus the electric field effectively, the electrodes need to be in contact with the patient at both the periphery and center of the wound itself. Since these wounds can be asymmetrical and deep, you need electrodes that can conform to a wide variety of surface features.”
“We tested the wound dressings in diabetic mice, which are a commonly used model for human wound healing,” Jakus added. “We found that the electrical stimulation from the device sped up the rate of wound closure, promoted new blood vessel formation, and reduced inflammation, all of which point to overall improved wound healing.”

Join the Community
Whether you’re an experienced professional or just starting your career, ASME’s membership community, resources and tools can help you with your lifelong journey.
Bandodkar said that what surprised and pleased him the most about the research was the effectiveness of the electric field in the bandages.
“We were concerned that the unregulated electrical field generated by our bandage would not provide impressive healing outcomes,” he said. “Prior work on electrical field-based wound healing relied on well-regulated fields using bulky electronics. To our surprise, not only did our bandages accelerate healing, the healing rates of our low-cost bandages were comparable to those achieved using expensive biologics.”
Another key factor is that WPEDs can be produced at relatively low cost. “We’re talking about a couple of dollars per dressing in overhead costs,” said Bandodkar.
The bandages can also be applied quickly and easily—this functionality enables patients to treat themselves at home, meaning they will be more likely to comply with treatment.
“Next steps for us include additional work to fine-tune our ability to reduce fluctuations in the electric field and extend the duration of the field,” said Bandodkar. “We are also moving forward with additional testing that will get us closer to clinical trials and, ultimately, practical use that can help people.”
Mark Crawford is a technology writer in Corrales, N.M.