Smart Bandage Does It All
Smart Bandage Does It All
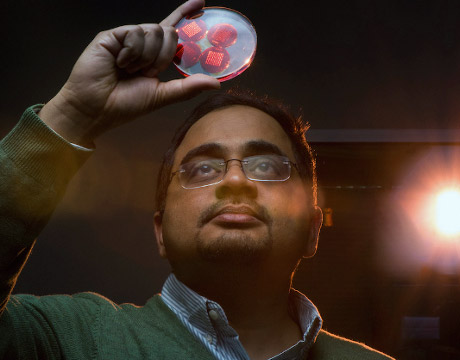
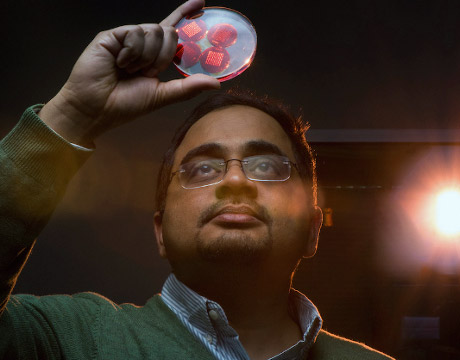
Prof. Sameer Sonkusale. Image: Tufts University
In another example of how technology continues to transform healthcare, engineers at Tufts University have developed “smart bandages” that can actively monitor and deliver precisely targeted treatment to chronic wounds while also keeping the caregiver informed of the patient’s progress.
Chronic wound treatment is a significant burden to patients and costly for the U.S. healthcare system, exceeding $20 billion each year.
The bandages have been engineered to track wound healing markers such as pH, temperature, oxygenation, and inflammatory molecules, and then electronically deliver drugs to treat the wound and improve the healing process. The bandages have been tested in the lab and are now undergoing pre-clinical studies.
For You: Mini Sensor Detects and Measures What We Eat
In a recent paper for Small, Prof. Sameer Sonkusale of Tufts University’s School of Engineering and his team wrote that the problem with some existing dressings that cover wounds and release therapeutic molecules passively is that they typically do not provide much information about the state of the healing process. The patients, therefore, need to be continuously monitored by medical professionals.
In the past, Sonkusale’s lab has made a variety of bandages that detect different conditions, target medication to a wound, and more. The new bandage combines much of that past work. “So with this, we’ve managed to put all of that together,” Sonkusale says.
The biggest engineering obstacle was how do we integrate all the different components into one [bandage] that maintains flexibility.Prof. Sameer Sonkusale, Tufts University
It’s a combination of five or six years of work that started with a National Science Award to fund work in flexible bioelectronics, an emerging area with broad implications in advancing basic life sciences and providing new tools for many clinical applications. Chronic wound management is one of the key application areas for flexible biomedical systems.
His smart bandage system is made of multiple components, including sensors for pH and temperature, a microheater, thermo-responsive drug carriers embedded in a hydrogel patch, and wireless electronics that read data from the sensors and control the thermal actuation system for automatically releasing drugs.
One patch includes the sensors, drug carrier, and microheater. When the pH of a chronic wound changes from acidic to alkaline, that typically indicates a bacterial infection. The temperature sensor also provides useful information about the level of inflammation in and around the wound.
A separate patch, or module, includes the electronics that records the sensors’ signals and powers the heater if needed, which in turn releases the appropriate amount of drug. The two sit side-by-side on a piece of transparent medical tape to form a flexible bandage less than 3-mm thick that is secured onto skin. The electronics patch is reusable after the other bandage patch is discarded.
This has all been made possible by the emergence of flexible electronics, flexible fabrication, flexible screen printing, and advancements in hydrogels and biomaterials, Sonkusale says. While flexible electronics have made many wearable medical devices possible, not much work has resulted in smart bandages, he says.
Sonkusale’s idea was to transform what has been a passive aid into a more active device that could help reduce the number of trips a patient takes to a healthcare facility, and to identify and address issues at an early stage with limited patient or caregiver involvement. People with certain conditions such as diabetes, those who have suffered traumatic injuries and burns, as well as the elderly are at particular risk for chronic wounds. Those are generally defined as wounds that don’t progress through the normal stages of healing and show no significant progress in a month. The immune system, which helps control inflammation, also becomes weaker as people age.
“The biggest engineering obstacle was how dowe integrate all the different components into one that maintains flexibility,” Sonkusale says. “There were a lot of challenges to make them flexible and able to be applied to the skin.”
The first step the team tackled was making a list of the various components thought should be part of the package. The most important consideration was the flexibility and biocompatibility of the bandage. From a practical standpoint, components were also selected to keep the bandage low cost and disposable. That was achieved in part by using screen printing and not having to work inside a clean room. “We don’t use expensive equipment,” he says.
According to the team’s paper, local targeted delivery of antibiotics is preferred over oral and topical treatment because it delivers precise and controlled administration, requires a smaller dose, and prevents damage to nearby healthy tissue. The wireless communication of data also keeps caregivers informed remotely.
Nancy S. Giges is an independent writer.
Read More:
Targeting Cancer Drugs to 3D-Printed Tumors
Engineers Contain Cancer Cells
MRI-Safe Robots Treat Epilepsy