Bioengineering Blog: Computational Modeling’s Place in Medical Device Testing
Bioengineering Blog: Computational Modeling’s Place in Medical Device Testing
The analysis of performance around diseased tissue can be used in very early research and development stages by using modeling and simulation in the design process.
Last month, I wrote a blog post about how computational modeling and simulation in medical device development is not a replacement for physical testing. But, there are areas where simulation can open new insights and opportunities compared to physical tests alone, whether bench testing in a laboratory or clinical trials in a hospital setting.
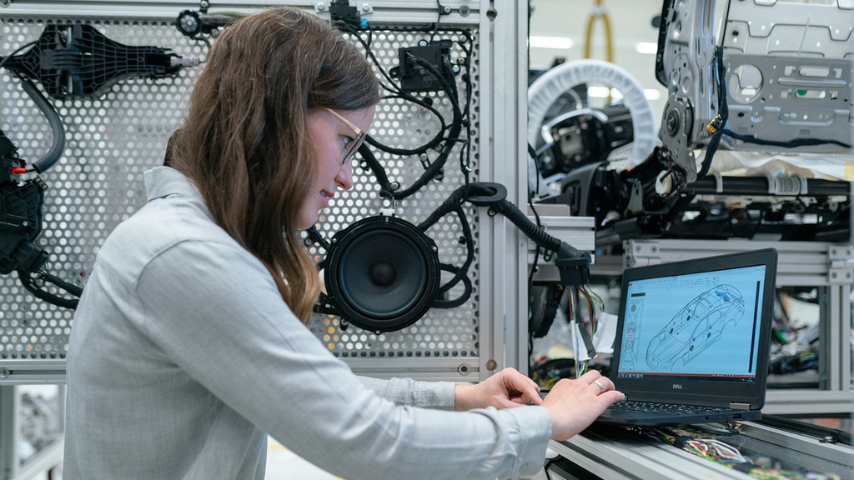
In a preclinical or clinical setting, there is a shift from the traditional method of building physical prototypes and performing tests to one that uses computational modeling and simulation as a parallel analysis and optimization path. This enables a product development team to gain insights in areas that are often not feasible through physical testing alone. From predicted performance in human patients with the expected disease states or across a wide demographic, there are clear advantages to updating the engineering development of medical devices to include in silico trials alongside the in vitro and in vivo testing.
Editor's Pick: Bioengineering Blog: Simulation at the Crossroads of Engineering and Biology
Early testing of prototypes has traditionally focused on bench models of healthy tissue. This makes sense from a cost and accessibility perspective, but the purpose of most medical devices is to treat a disease in one form or another. These disease states change the properties and response of target tissues, but testing physical models that mimic these changes can be expensive and time-consuming to implement. By incorporating computational modeling and simulation into the design process, it is possible to bring the analysis of performance around diseased tissue to very early research and development stages. With information on how the anatomy and physiology change with disease progression, the design can be optimized for the intended end use case.
Another benefit of including simulation as part of the medical device development process is the ability to model larger, more diverse patient populations earlier. Clinical trials are expensive and time-consuming and are therefore scheduled late in the development of the devices. If safety or efficacy issues are highlighted at this stage, the choice is to go back and make design changes or restrict the indications for use to a smaller patient population. Design changes get more expensive by orders of magnitude compared to the early concept phases, so the latter is often the result.
More for You: Bioengineering Blog: An Emerging Regulatory Framework for Medical Device Simulation
With modeling and simulation, it is possible to look at a more comprehensive patient population while still in the early, less expensive stages of development. This allows for the changes necessary to make sure the device and treatment are effective across the entire patient population and adds to the understanding of how that treatment changes with different patients. Additionally, with the reduced cost associated with evaluating patent populations, the financial feasibility bar is lowered enough to make treatments available to rarer diseases that would have previously needed to compromise with a less ideal procedure.
To find truly innovative solutions to the complex problems facing patient treatment today, there is a real need to increase the speed of analysis and reduce the cost when exploring the edge cases. So much of innovation is taking an initial idea and using testing to learn from the insights along the way that help inform the decisions that optimize a medical device to be effective for the largest patient population possible while reducing the cost of development.
Arlen Ward, Ph.D., P.E., is a Principal Modeling and Simulation Engineer with System Insight Engineering LLC, a medical device simulation consultancy.
Opinions expressed are the author’s and do not necessarily reflect the views of ASME.
In a preclinical or clinical setting, there is a shift from the traditional method of building physical prototypes and performing tests to one that uses computational modeling and simulation as a parallel analysis and optimization path. This enables a product development team to gain insights in areas that are often not feasible through physical testing alone. From predicted performance in human patients with the expected disease states or across a wide demographic, there are clear advantages to updating the engineering development of medical devices to include in silico trials alongside the in vitro and in vivo testing.
Editor's Pick: Bioengineering Blog: Simulation at the Crossroads of Engineering and Biology
Early testing of prototypes has traditionally focused on bench models of healthy tissue. This makes sense from a cost and accessibility perspective, but the purpose of most medical devices is to treat a disease in one form or another. These disease states change the properties and response of target tissues, but testing physical models that mimic these changes can be expensive and time-consuming to implement. By incorporating computational modeling and simulation into the design process, it is possible to bring the analysis of performance around diseased tissue to very early research and development stages. With information on how the anatomy and physiology change with disease progression, the design can be optimized for the intended end use case.
Another benefit of including simulation as part of the medical device development process is the ability to model larger, more diverse patient populations earlier. Clinical trials are expensive and time-consuming and are therefore scheduled late in the development of the devices. If safety or efficacy issues are highlighted at this stage, the choice is to go back and make design changes or restrict the indications for use to a smaller patient population. Design changes get more expensive by orders of magnitude compared to the early concept phases, so the latter is often the result.
More for You: Bioengineering Blog: An Emerging Regulatory Framework for Medical Device Simulation
With modeling and simulation, it is possible to look at a more comprehensive patient population while still in the early, less expensive stages of development. This allows for the changes necessary to make sure the device and treatment are effective across the entire patient population and adds to the understanding of how that treatment changes with different patients. Additionally, with the reduced cost associated with evaluating patent populations, the financial feasibility bar is lowered enough to make treatments available to rarer diseases that would have previously needed to compromise with a less ideal procedure.
To find truly innovative solutions to the complex problems facing patient treatment today, there is a real need to increase the speed of analysis and reduce the cost when exploring the edge cases. So much of innovation is taking an initial idea and using testing to learn from the insights along the way that help inform the decisions that optimize a medical device to be effective for the largest patient population possible while reducing the cost of development.
Arlen Ward, Ph.D., P.E., is a Principal Modeling and Simulation Engineer with System Insight Engineering LLC, a medical device simulation consultancy.
Opinions expressed are the author’s and do not necessarily reflect the views of ASME.